In This Article
Genetic hearing loss can feel daunting, yet understanding the science—and the human stories behind it—offers real hope. This guide explains why certain gene changes affect hearing, how testing works, and the many ways you can thrive with the right support.

Understanding Genetic Hearing Loss
Genes carry blueprints that tell every ear cell how to build, connect, and send sound to your brain. When small DNA changes disrupt those instructions, you can be born with hearing loss or notice it later in life.
Most genetic faults harm the fragile hair cells in the inner ear or the nerve fibers that carry sound. Loud noise, infections, or certain antibiotics can add to the damage, so genes and environmental factors often work together.
Families usually meet two broad categories:
Sound waves travel through the ear canal, make the eardrum vibrate, and move three tiny middle-ear bones. Vibrations then reach the cochlea—an inner-ear spiral filled with fluid and hair cells that translate motion into nerve impulses your brain understands as music, speech, or a baby’s laugh.
When genes that guide any step of this chain malfunction, signals fade or disappear. That is why some people notice only mild trouble hearing birdsong, while others never detect speech at all.
A quick orientation helps you discuss results with doctors:
Maria’s parents learned she had profound deafness at two weeks old through newborn screening. A genetic panel later showed two changes in her GJB2 gene. Knowing the cause guided her family toward early cochlear implantation and speech therapy, letting Maria start kindergarten using spoken English and American Sign Language. Her story reminds us that genes provide information—not limitations.
Genes travel through families in predictable “traffic patterns.” Understanding these patterns helps you gauge risk and talk with relatives.
| Pattern | Who Can Pass It On? | Typical Onset | Family Clues |
| Autosomal recessive | Both parents (carriers) | Birth or early childhood | Often no prior deaf relatives |
| Autosomal dominant | Either parent (affected) | Childhood to mid-life | Multiple generations with progressive loss |
| X-linked | Carrier mother or affected father | Birth – childhood (males) | Affects mostly sons |
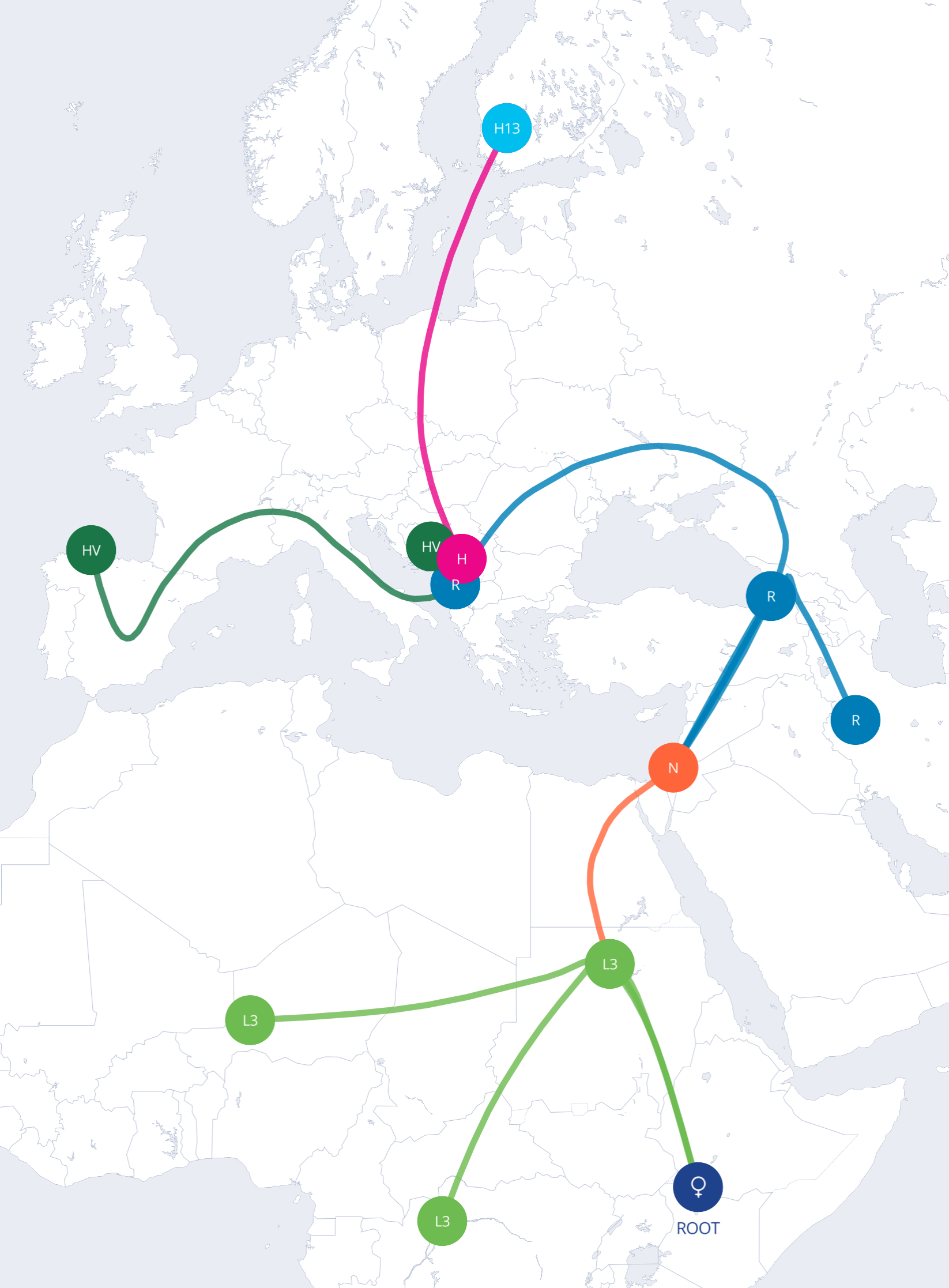
| Mitochondrial | Affected mother | Any age; may worsen with certain drugs | Both sons and daughters affected, but only daughters pass it on |
Even within one family, an identical mutation can cause mild loss in one person and profound loss in another. Doctors call this variable expressivity. Sometimes a person carries a change but never develops symptoms—a concept known as incomplete penetrance. Recognizing these nuances eases guilt and blame when relatives compare experiences.
Jordan’s grandfather used bulky hearing aids by age 40, yet Jordan’s mother hears well in quiet rooms. Genetic testing revealed the same KCNQ4 mutation in both. Their audiologist explained that lifestyle factors—like decades of factory noise for Grandpa—can tilt gene effects toward worse outcomes, reinforcing the value of early protection.
Some genes pop up again and again in clinics worldwide:
Knowing which gene is involved shapes medical choices. For instance, children with OTOF changes often benefit dramatically from early cochlear implants because their hearing nerve remains healthy.
Know Your DNA Reviews

Don't miss out on the opportunity to learn more about yourself. Read our best DNA test page to find the best one for you.
Testing helps families move from “why?” to clear answers and practical next steps. Doctors recommend it when hearing loss:
A typical evaluation begins with a physical exam, hearing tests, and imaging if needed. If clues point to a genetic cause, your clinician may order a comprehensive gene panel that reads dozens of hearing-loss genes at once. These panels catch roughly 40–50 % of genetic cases—far more than single-gene tests of the past.
The process is straightforward:
Many insurers cover testing when a specialist documents medical need. If cost feels overwhelming, ask your clinician about patient-assistance programs or research studies that include free testing.
Hearing your DNA story can stir relief, fear, or both. Counselors respect these emotions, translate jargon, and help you share information with relatives. You can find a certified genetic counselor online through the National Society of Genetic Counselors.
Genes set the stage, but timely care writes the storyline. Early intervention gives the brain rich sound input during critical language windows.
Modern digital aids fit infants as young as four weeks. They amplify speech selectively, reduce background noise, and pair with phones or classroom microphones. Families often try hearing aids first, even for severe loss, to see how much benefit remains.
When hair cells are too damaged, cochlear implants bypass them entirely. Surgeons thread a tiny electrode array into the cochlea, then external processors convert sound into electrical signals that stimulate the auditory nerve. Children implanted before 12 months often reach age-appropriate language milestones.
Research shows implants work especially well for kids whose deafness stems from GJB2 or OTOF mutations, because their nerve pathways stay intact. Outcomes vary with age at surgery, therapy intensity, and individual brain plasticity.
Experienced therapists teach listening skills, spoken language, and strategies for noisy settings. Even teens and adults gain from targeted training apps that sharpen speech discrimination.
Early-hearing-detection programs connect families to audiologists, therapists, and parent mentors. These networks help you navigate insurance, choose communication modes, and prepare for school transitions.
| Current Option | How It Helps Today | What’s Coming Next |
| Hearing aids | Amplify remaining hearing; quick, non-surgical | Smarter AI processing, rechargeable micro-devices |
| Cochlear implants | Provide sound sensation when hair cells fail | Fully implantable processors; music-quality upgrades |
| Auditory-brainstem implants | Bypass cochlea for rare nerve absence | Refined electrode patterns for clearer speech |
| Gene therapy | Experimental inner-ear delivery of healthy genes | Wider gene targets; one-time treatments in childhood |
In January 2024, surgeons at Children’s Hospital of Philadelphia lifted a tiny flap of a child’s eardrum and infused healthy OTOF genes through the round window membrane. Months later, the patient detected soft voices and environmental sounds for the first time.
A June 2024 multi-center trial reported that five formerly deaf children gained speech recognition after similar procedures. While still experimental, these milestones signal a future where correcting the root cause may replace lifelong devices for some families.
Safety questions remain: How long will the benefit last? Could immune reactions arise? Researchers monitor participants closely, but early glimpses are encouraging.
A genetic diagnosis touches identity, family ties, and daily life far beyond decibel levels. Facing that reality with empathy empowers you to shape a fulfilling narrative.
Early Individualized Education Programs (IEPs) provide classroom amplification systems, captioned videos, and extra processing time. Adults can request reasonable accommodations—like captioned meetings or vibrating alerts—under the Americans with Disabilities Act.
Families may choose spoken language, American Sign Language (ASL), cued speech, or a bilingual approach. None is “better”; the right mix depends on your child’s needs and family culture. Many people fluent in ASL thrive within Deaf culture while also using technology to stay flexible in mixed settings.
Whether you identify as a Deaf individual, a person with hearing loss, or something in between, genetics does not define your worth. Community, creativity, and resilience often flourish in spaces where sound once felt scarce.
Knowing the cause of hearing loss is only the beginning. A few practical moves can turn that knowledge into action.
Remember, genetics provides clarity—not destiny. With timely care, community, and emerging therapies, you can craft a rich life filled with connection and sound in all its forms.
Know Your DNA Reviews
Looking for a DNA test that's accurate and can tell you about your health and heritage?
